

The settings included general practice clinics (n=18), specialized care units (n=14), and emergency and ambulatory units (n=3). Of the 1,907 records retrieved, 35 studies met the inclusion criteria. Independent reviewers screened abstracts, read full texts, extracted data from the included studies, and appraised methodological quality assessments. This study was conducted in order to provide a critical appraisal and synthesize the best available evidence on the impact of implementing clinical microsystem (CMS) on quality of care and safety of the health care delivery.Ī comprehensive and systematic search of six electronic databases, from 1998 to 2018, was conducted to identify empirical literature published in both English and French, evaluating the impact of implementing CMS in healthcare settings. There is currently no other empirical studies within the academic literature which investigate the value of the clinical microsystems approach to an English NHS context.įaced with the increased expectations on the quality and safety of health care delivery systems, a number of stakeholders are increasingly looking for more efficient ways to deliver care. In particular, the importance of strong data collection in achieving "high performing" status is emphasised. This sample represented sites of different sizes, coverage of primary, secondary and tertiary care and those reporting more and less positive experiences of the clinical microsystems approach-but any findings may be limited in their generaliseability and further studies may be needed to test out the relevance of these findings in wider settings.įuture microsystem programmes will need to address components of patient involvement and process/outcome monitoring if the broader legitimacy of the approach is to be cemented and enhanced. The evaluation was limited in terms of the numbers of case study sites that it was able to incorporate.
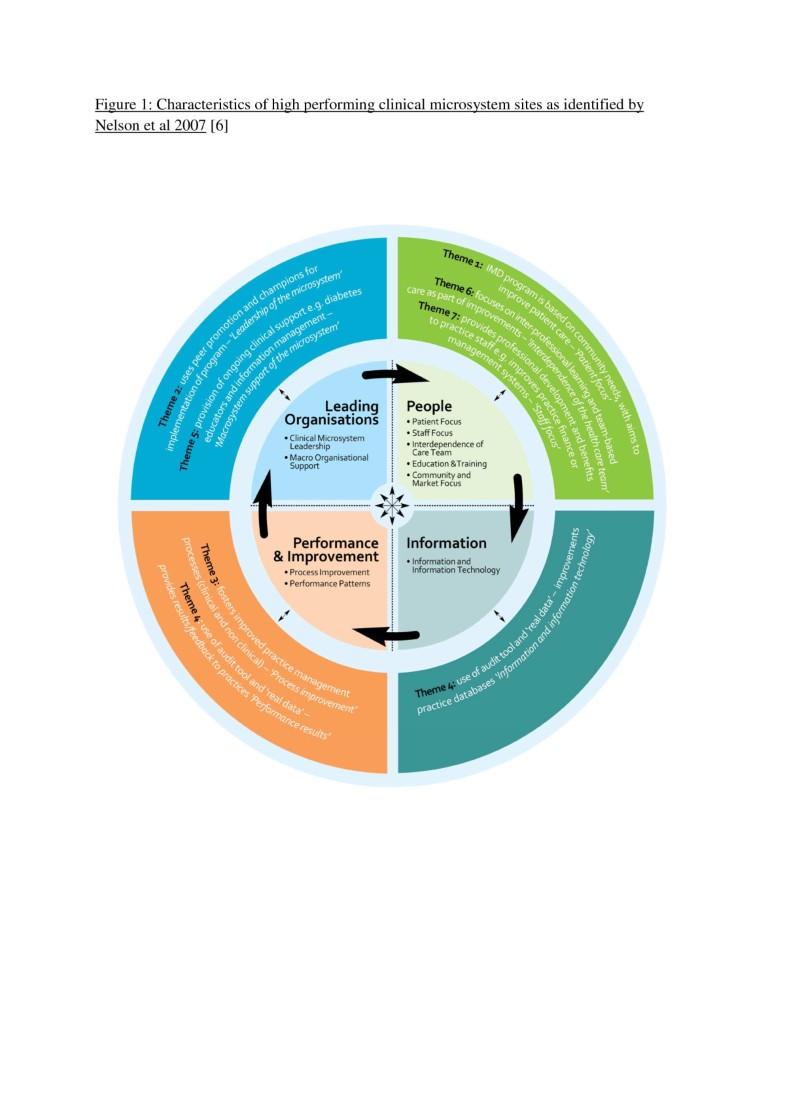
To a lesser extent the research also indicated an enhanced predisposition towards improvement and innovation and a seemingly embedded sense of improvement as an ongoing (if essentially episodic) process. The case study sites demonstrated higher staff morale, empowerment, commitment and clarity of purpose. The clinical microsystem approach emphasises identifying and nurturing strengths-of both teams and individuals-and this reinforced these positive aspects. The research concurred with many of the claims for clinical microsystems, particularly that democratic, consensual approaches to change and improvement can be better received than externally derived initiatives with imposed targets. Data was triangulated to produce case studies for each of the sites. Interviews and group discussions were used to collect qualitative data, whist quantitative outcome data was also collected within each of the sites. The research adopted a Realistic Evaluation approach to examine a series of pilot clinical microsystems sites to determine what worked for whom, when and within what circumstances.

The purpose of this paper is to evaluate the claims made for the clinical microsystems approach of healthcare improvement within an English NHS context.


 0 kommentar(er)
0 kommentar(er)
